When Ravi, a 42-year-old software engineer from Delhi, was diagnosed with Type 2 diabetes, he was initially overwhelmed by the dietary changes and regular monitoring his doctor recommended. However, over time, he found a rhythm: he ate a balanced diet, exercised regularly, and managed to keep his HbA1c in the target range.
Everything seemed to be under control until a routine blood test revealed shockingly high cholesterol levels. Ravi was stunned. “I’ve been doing everything right,” he told his doctor. “Why is this happening?”
His friend Suresh, also diabetic, never seemed to worry about cholesterol at all. “My reports are always normal,” Suresh said. “Maybe it’s just bad luck for you.” But Ravi wasn’t convinced — it felt like there had to be more to the story. Let’s dive into the facts associated with such instances.
A Puzzling Reality
Diabetics like Ravi often find themselves puzzled by cholesterol issues, especially when their peers with similar conditions don’t face the same challenges. You might wonder why does one diabetic patient develop high cholesterol levels while another’s levels remain normal?
The answer to this question lies in a complex interplay of genetics, lifestyle, and even the type of diabetes. High cholesterol in diabetics isn’t just a side effect of the condition, instead, it’s influenced by multiple factors that vary drastically from one individual to another. Let’s have a look at some of these factors.


1. The Role of Genetics: What’s in Your DNA?
For Ravi, it turned out that genetics played a major role. After consulting a diabetes specialist, he was diagnosed with familial hypercholesterolemia (FH), a genetic condition that predisposes people to high cholesterol regardless of lifestyle.
Genetics can influence the way your body processes fats. Some diabetics inherit a predisposition to produce too much LDL (bad cholesterol in simpler terms) or too little HDL (good cholesterol in simpler terms). This is why even a healthy lifestyle may not completely prevent high cholesterol in some individuals.
Ravi was relieved to learn it wasn’t his fault but also frustrated by the realization that he’d need medication in addition to lifestyle changes. “I thought managing diabetes was hard enough,” he said, “but now there’s more to handle.”
2. Type of Diabetes Matters: Type 1 vs. Type 2
Ravi’s doctor explained that Type 1 and Type 2 diabetes don’t affect cholesterol in the same way. Type 2 diabetes is often accompanied by metabolic syndrome, which includes high triglycerides, low HDL, and elevated LDL in most patients.
Here is the report of Ravi a year after his diabetes was diagnosed. At this stage, his HBA1C was in prediabetic range but the cholesterol levels were higher than normal. Note that the names of the patient and other personally identifiable information have been changed to maintain patient privacy.
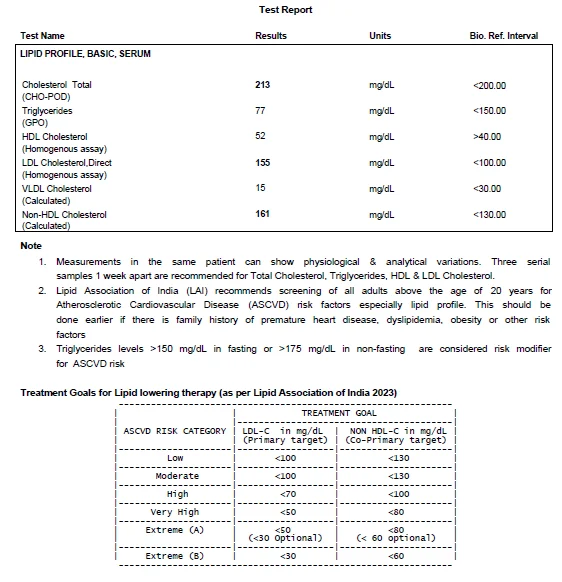
On the other hand, Type 1 diabetics might develop cholesterol issues later in life due to prolonged insulin therapy or complications like chronic kidney disease. In Ravi’s case, his Type 2 diagnosis came with an increased risk of dyslipidemia — a condition where abnormal cholesterol levels are almost inevitable without intervention.
3. Hidden Triggers: Silent Culprits in Everyday Life
Even with a healthy diet and regular exercise, there might still be gaps in your routine that you may not realize initially. As an example, someone’s love of sugary tea and frequent use of butter in cooking can add hidden fats and sugars to their diet. These small indulgences accumulate over time which contribute to high cholesterol levels.
Stress can be another silent culprit. You may often work late hours, skipping meals and overindulging in comfort foods when you finally sat down to eat. Stress hormones like cortisol can increase cholesterol levels and disrupt blood sugar control, making the situation even worse.

4. Medications: Helping or Hurting?
During a follow-up visit, Ravi’s doctor reviewed his medications and pointed out a possible issue. Some diabetes drugs, such as thiazolidinediones, can increase LDL cholesterol. Ravi wasn’t aware that managing one condition could sometimes complicate another. His doctor adjusted his medications, adding a statin to manage his cholesterol.
“Why didn’t anyone warn me about this earlier?” Ravi wondered. His doctor explained that not all patients experience medication-related cholesterol changes, but for those who do, it’s important to identify and address the issue early.
5. The Gut-Cholesterol Connection
This is one of the most surprising revelations. Research shows that the gut microbiome —trillions of bacteria in the digestive system — also plays a major role in cholesterol metabolism.
Foods that are rich in probiotics, such as yogurt, and prebiotics, like fiber-rich vegetables, can improve gut health and help regulate cholesterol.
A Plan That Works for You
After months of trial and error, Ravi began to see improvements in his cholesterol levels. His LDL came down, his HDL went up, and his triglycerides stabilized. The key wasn’t just in one magical solution but in understanding how his unique body worked and addressing the specific factors that affected him.
Ravi’s journey taught him that cholesterol management isn’t one-size-fits-all, especially for diabetics. Genetics, medication, diet, and even stress levels all play a role. “It’s not fair to compare myself to Suresh anymore,” Ravi admitted. “We’re dealing with completely different challenges.”
Takeaway for Others
If you’re diabetic and struggling with cholesterol, remember that your experience is unique. Factors like family history, the type of diabetes you have, and even subtle lifestyle habits can influence your cholesterol levels.
Work closely with your healthcare team to identify what’s behind your numbers. Be proactive, ask about genetic testing, medication adjustments, or new dietary approaches. Small, personalized changes can lead to big results, just like they did for Ravi.
Every diabetic’s journey with cholesterol is different, but understanding your body’s needs is the first step toward better health.