Living with diabetes can be a challenging journey, not only for individuals diagnosed with the condition but also for their caregivers. Diabetes is a chronic metabolic disorder characterized by high blood sugar levels, and it affects millions of people worldwide. While managing diabetes is already demanding, a more significant concern arises from the relationship between diabetes, hypertension, and heart disease, forming a vicious triad that can severely impact the quality of life of diabetic patients. In this article, we will explore the interconnections between these three conditions, the risks they pose, and essential strategies to manage them effectively.
Understanding Diabetes, Hypertension, and Heart Disease
Diabetes: Diabetes mellitus is a metabolic disorder caused by the body’s inability to produce enough insulin or properly use insulin to regulate blood sugar levels. It is classified into type 1 diabetes (insulin-dependent) and type 2 diabetes (non-insulin-dependent).
Diabetes occurs when the pancreas fails to produce sufficient insulin or when the body’s cells become resistant to insulin. Insulin is a hormone responsible for facilitating the entry of glucose from the bloodstream into cells, where it is used for energy. In diabetes, glucose accumulates in the blood, leading to high blood sugar levels, a condition known as hyperglycemia.
Type 1 diabetes is an autoimmune condition where the immune system mistakenly attacks and destroys insulin-producing cells in the pancreas. It typically develops in childhood or early adulthood and requires lifelong insulin therapy.
Type 2 diabetes is more common and often linked to lifestyle factors, such as unhealthy diet and lack of physical activity. While the pancreas may still produce insulin in type 2 diabetes, the body’s cells become resistant to its effects, making it difficult for glucose to enter the cells.
Hypertension: Hypertension, commonly known as high blood pressure, is a condition where the force of blood against the artery walls is consistently too high. It is often referred to as the “silent killer” as it may not present noticeable symptoms initially.
Blood pressure is measured using two values: systolic pressure (the higher value) represents the pressure in the arteries when the heart contracts, and diastolic pressure (the lower value) is the pressure when the heart relaxes between beats. Normal blood pressure is typically around 120/80 mmHg.
Hypertension is diagnosed when blood pressure consistently exceeds 130/80 mmHg. If left untreated, high blood pressure can strain the heart and blood vessels, increasing the risk of heart disease, stroke, and kidney problems.
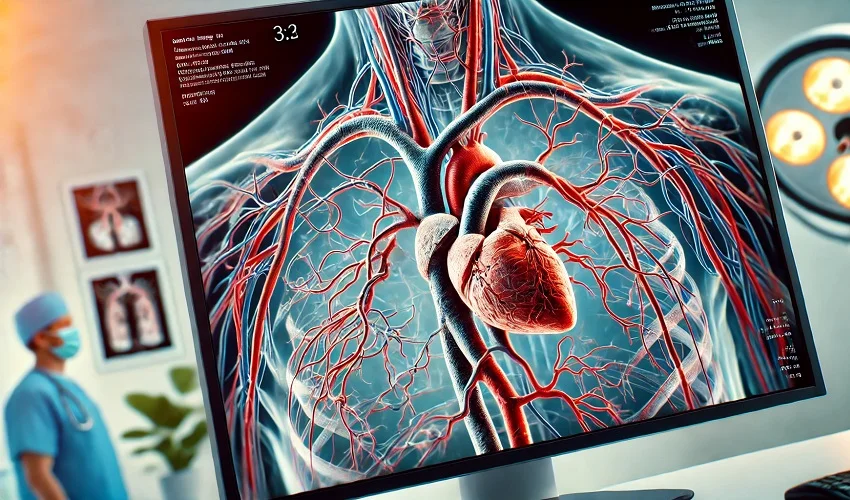
Heart Disease: Heart disease encompasses various conditions that affect the heart, including coronary artery disease, heart failure, and arrhythmias. It is a leading cause of death globally. Coronary artery disease (CAD) occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of plaque (atherosclerosis). This restricts blood flow to the heart and can lead to angina (chest pain) or a heart attack.
Heart failure occurs when the heart is unable to pump blood effectively, causing fatigue, shortness of breath, and fluid retention.
Arrhythmias are abnormal heart rhythms that can be too fast, too slow, or irregular, potentially leading to palpitations, dizziness, or fainting.
The Vicious Triad: Interconnection Between Diabetes, Hypertension, and Heart Disease
Shared Risk Factors: Diabetes, hypertension, and heart disease share several risk factors, such as obesity, sedentary lifestyle, unhealthy diet, family history, and age.
Obesity is a significant risk factor for all three conditions. Excess body weight can contribute to insulin resistance in diabetes, strain the cardiovascular system in hypertension, and increase the workload on the heart, leading to heart disease.
A sedentary lifestyle and lack of physical activity are associated with a higher risk of diabetes, hypertension, and heart disease. Regular exercise helps improve insulin sensitivity, lower blood pressure, and maintain heart health.
An unhealthy diet, especially one high in processed foods, sugary beverages, and saturated fats, can contribute to the development of diabetes, hypertension, and heart disease. A diet rich in fruits, vegetables, whole grains, and lean proteins is recommended for prevention and management.
A family history of diabetes, hypertension, or heart disease can increase an individual’s susceptibility to these conditions. Genetic factors play a role in their development.
Age is a non-modifiable risk factor, as the risk of developing diabetes, hypertension, and heart disease tends to increase with age.
Impact of Diabetes on Hypertension: Diabetes can damage blood vessels and the kidneys, leading to increased blood pressure. Additionally, high blood sugar levels may contribute to arterial stiffness, exacerbating hypertension.
Uncontrolled diabetes can lead to damage to the inner lining of blood vessels, called the endothelium. This endothelial dysfunction can impair the blood vessels’ ability to relax and contract, contributing to hypertension.
Diabetes can also affect the kidneys, leading to diabetic nephropathy, a condition where the kidneys’ filtering units become damaged. As the kidneys play a crucial role in regulating blood pressure, kidney dysfunction can lead to hypertension.
Chronic hyperglycemia in diabetes can cause the formation of advanced glycation end-products (AGEs), which can stiffen and narrow the arteries, increasing blood pressure.
Impact of Hypertension on Diabetes: Hypertension can worsen insulin resistance, making blood sugar control more challenging for diabetic individuals. Furthermore, some antihypertensive medications can affect blood sugar levels.
High blood pressure is associated with insulin resistance, meaning the body’s cells are less responsive to insulin’s actions. This can result in poorer glucose uptake by cells, leading to elevated blood sugar levels in diabetic patients.
Certain classes of antihypertensive medications, such as beta-blockers and thiazide diuretics, may interfere with glucose metabolism and worsen blood sugar control. However, not all antihypertensive drugs have this effect, and healthcare providers can choose medications that are less likely to impact blood sugar levels.
Diabetic Heart Disease: Diabetes increases the risk of developing heart disease significantly. Diabetic patients are more prone to coronary artery disease and have a higher likelihood of experiencing heart attacks.
The high levels of blood sugar in diabetes can damage blood vessels, promoting the development of atherosclerosis (plaque buildup) in the coronary arteries. This condition, known as coronary artery disease, narrows the arteries and restricts blood flow to the heart muscle, increasing the risk of heart attacks.
Diabetic patients are also more susceptible to silent heart attacks, which may go unnoticed as they may not experience typical chest pain symptoms.
The Risks and Complications of the Vicious Triad
Cardiovascular Complications: The combination of diabetes, hypertension, and heart disease significantly raises the risk of cardiovascular complications, including strokes, heart attacks, and peripheral artery disease.
A stroke occurs when the blood supply to a part of the brain is disrupted, either due to a blood clot (ischemic stroke) or a ruptured blood vessel (hemorrhagic stroke). Diabetes and hypertension increase the risk of stroke, and the presence of heart disease further compounds this risk.
Heart attacks, also known as myocardial infarctions, result from a sudden blockage of blood flow to the heart muscle. Diabetic patients with hypertension have a higher likelihood of experiencing heart attacks due to the combined effects of atherosclerosis and increased cardiac workload.
Peripheral artery disease (PAD) is a condition where blood flow to the legs and feet is reduced due to narrowed arteries. Diabetic patients with hypertension are at a higher risk of developing PAD, which can lead to pain, non-healing wounds, and even limb amputation.
Kidney Disease: Diabetes and hypertension are the leading causes of chronic kidney disease. The vicious triad puts diabetic patients at an even higher risk of kidney damage and kidney failure. Diabetic nephropathy is a specific type of kidney disease caused by diabetes. Over time, high blood sugar levels can damage the delicate filtering units in the kidneys (glomeruli), leading to proteinuria (excess protein in urine) and a decline in kidney function.
Hypertension can independently cause kidney damage by straining the blood vessels within the kidneys. When combined with diabetes, the risk of kidney complications is substantially increased.
Chronic kidney disease can progress to end-stage renal disease (ESRD), where the kidneys are no longer able to filter waste products from the blood effectively. Patients with ESRD require dialysis or kidney transplantation to survive.
Neuropathy: Diabetes, particularly when uncontrolled, can lead to nerve damage (neuropathy). This, coupled with reduced blood flow due to hypertension and heart disease, may result in severe complications like diabetic foot ulcers.
Diabetic neuropathy is a common complication of diabetes that affects the nerves throughout the body. Peripheral neuropathy affects the nerves in the extremities, leading to symptoms such as tingling, numbness, and pain in the feet and hands.
Reduced blood flow to the extremities, a consequence of hypertension and atherosclerosis, further exacerbates neuropathic symptoms.
Diabetic foot ulcers can develop when neuropathy causes a loss of sensation in the feet, leading to injuries or wounds going unnoticed. Combined with poor circulation, these ulcers can be difficult to heal and may lead to serious infections or even amputation.
Retinopathy: Uncontrolled diabetes can lead to retinopathy, a condition where the blood vessels in the retina are damaged. Hypertension further contributes to retinal problems, leading to vision impairment or even blindness.
The retina is the light-sensitive layer at the back of the eye that plays a crucial role in vision. High blood sugar levels can cause damage to the small blood vessels in the retina, leading to diabetic retinopathy.
Hypertension can further damage the blood vessels in the eyes, exacerbating retinopathy and increasing the risk of vision loss.
Diabetic retinopathy can progress to more severe stages, such as proliferative retinopathy, where abnormal blood vessels grow in the retina. If left untreated, these vessels can leak and cause retinal detachment, resulting in permanent vision loss.
Managing the Vicious Triad: Strategies for Diabetic Patients and Caregivers
Regular Monitoring: Regular monitoring of blood sugar, blood pressure, and cholesterol levels is crucial for effective management and early detection of any complications.
For diabetic patients, self-monitoring of blood glucose levels using a glucometer is essential in keeping blood sugar levels within a target range. Frequent testing can help identify patterns and guide treatment adjustments.
Blood pressure should be monitored regularly at home and during healthcare visits. Diabetic patients should aim to maintain their blood pressure below 130/80 mmHg, as recommended by medical guidelines.
Regular cholesterol checks are necessary to assess lipid levels, which can impact cardiovascular health. High levels of low-density lipoprotein (LDL) cholesterol are a risk factor for heart disease, while high levels of high-density lipoprotein (HDL) cholesterol are considered beneficial.
Lifestyle Modifications: Encouraging a healthy lifestyle is fundamental. This includes a balanced diet rich in vegetables, fruits, whole grains, lean protein, and healthy fats. Regular physical activity can also aid in controlling blood sugar and blood pressure.
A balanced diet is essential for managing diabetes and promoting heart health. A focus on whole, nutrient-dense foods can help control blood sugar and blood pressure levels.
Carbohydrate counting or the use of the glycemic index can help diabetic patients manage their blood sugar levels more effectively.
Physical activity, such as brisk walking, swimming, or cycling, is beneficial for diabetic patients and can help lower blood pressure. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week.
Medication Adherence: Diabetic patients with hypertension may be prescribed multiple medications. Adhering to the prescribed treatment plan is essential for optimal control of both conditions.
Diabetes management may involve various medications, including insulin, oral antidiabetic agents, or a combination of both. Adhering to the prescribed medication regimen is vital in maintaining stable blood sugar levels.
For hypertension, antihypertensive medications may include diuretics, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin receptor blockers (ARBs). Compliance with medication schedules is crucial in managing blood pressure effectively.
It is essential to communicate with healthcare providers about any concerns or side effects experienced with medications. They can help adjust the treatment plan, if necessary, to ensure better tolerability and adherence.
Stress Management: Chronic stress can adversely affect blood sugar and blood pressure levels. Practicing relaxation techniques like meditation or yoga can help in stress management.
Stress and anxiety can contribute to elevated blood sugar levels in diabetic patients, as well as temporarily raise blood pressure.
Mindfulness-based practices, such as meditation and deep breathing exercises, can help reduce stress and promote emotional well-being.
Engaging in hobbies, spending time with loved ones, and participating in enjoyable activities can also serve as effective stress-reducing measures.
Regular Checkups: Regular visits to healthcare professionals are essential to evaluate the effectiveness of the treatment plan and make any necessary adjustments.
Scheduled visits with healthcare providers allow for ongoing monitoring of blood sugar, blood pressure, and cholesterol levels.
Healthcare providers can assess the patient’s overall health, review the efficacy of medications, and provide education on managing the conditions effectively.
Regular checkups also offer opportunities to discuss any concerns or challenges faced in managing diabetes, hypertension, and heart disease.
The vicious triad of diabetes, hypertension, and heart disease presents a considerable challenge for diabetic patients and their caregivers. Understanding the interconnections between these conditions is crucial for effective management and reducing the risk of complications. By adopting a healthy lifestyle, adhering to prescribed medications, and maintaining regular checkups, diabetic patients can significantly improve their quality of life and mitigate the adverse effects of the triad. As caregivers, offering support, encouragement, and education can make a substantial positive impact on the lives of those living with diabetes. With proper management, it is possible to lead a fulfilling life despite the challenges posed by the vicious triad.