Living with type 2 diabetes can be a challenging journey, as the disease evolves over time and presents various changes and considerations. Understanding how type 2 diabetes progresses and what to expect along the way is crucial for both patients and caregivers in managing the condition effectively. In this article, we will delve into the intricate details of the progression of type 2 diabetes, exploring the various stages, symptoms, complications, and lifestyle modifications that can help maintain a high quality of life. By shedding light on this topic, we aim to provide valuable insights and educational information to empower diabetic patients and their caregivers.
Understanding Type 2 Diabetes: A Brief Overview
Type 2 diabetes is a chronic metabolic disorder characterized by elevated blood glucose levels due to insulin resistance or insufficient insulin production. It accounts for the majority of diabetes cases worldwide, affecting millions of individuals. According to the International Diabetes Federation, around 463 million people were living with diabetes in 2019, with type 2 diabetes comprising approximately 90% of these cases.
Type 2 diabetes is influenced by a combination of genetic and environmental factors. Key risk factors include obesity, sedentary lifestyle, unhealthy eating habits, family history of diabetes, age, and certain ethnic backgrounds. Modifying these risk factors can significantly reduce the risk of developing type 2 diabetes.
Progression of Type 2 Diabetes
Type 2 diabetes is a dynamic condition that progresses over time, and understanding its trajectory is essential for effectively managing the disease. The journey begins with the early stages, progresses to the onset of type 2 diabetes, and potentially leads to long-term effects and complications if left unmanaged. By unraveling the progression of type 2 diabetes, individuals and their caregivers can gain insights into the changes that occur and better prepare for what lies ahead.
Early Stages: Prediabetes
Prediabetes is a condition where blood glucose levels are higher than normal but not yet at the diabetic range. It serves as a warning sign and an opportunity for intervention to prevent or delay the onset of type 2 diabetes. Prediabetes is often asymptomatic, making regular screenings essential for early detection. Lifestyle modifications, such as adopting a healthy diet, increasing physical activity, and maintaining a healthy weight, can effectively manage prediabetes. Studies have shown that individuals with prediabetes who make these lifestyle changes can reduce their risk of developing type 2 diabetes by up to 58%.
Onset of Type 2 Diabetes
When prediabetes progresses, individuals may develop type 2 diabetes. The body’s cells become resistant to insulin, leading to inadequate glucose uptake and elevated blood sugar levels. Common symptoms at this stage include increased thirst, frequent urination, fatigue, and blurred vision. However, it is important to note that not everyone with type 2 diabetes experiences noticeable symptoms, and the condition may be detected through routine blood tests.
Long-term Effects and Complications
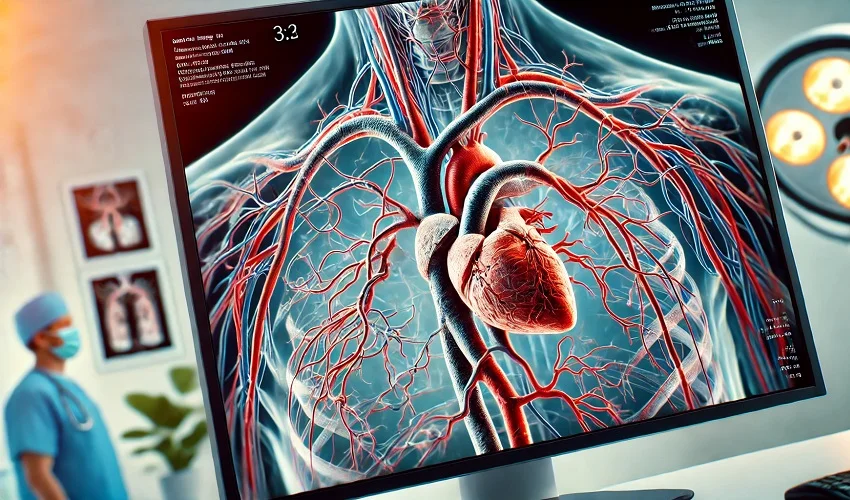
If left unmanaged, type 2 diabetes can lead to various long-term complications affecting multiple organ systems. These complications include cardiovascular diseases, neuropathy (nerve damage), nephropathy (kidney damage), retinopathy (eye damage), and increased susceptibility to infections. Controlling blood sugar levels, blood pressure, and cholesterol levels are essential in reducing the risk of these complications. Regular medical check-ups, blood sugar monitoring, and adherence to treatment plans are crucial in preventing or managing these complications.
Managing Type 2 Diabetes: Key Considerations
Successfully managing type 2 diabetes requires a comprehensive approach that encompasses various key considerations. By implementing these strategies, individuals can effectively control their blood sugar levels, reduce the risk of complications, and improve their overall quality of life.
Lifestyle Modifications
Adopting a healthy lifestyle is fundamental in managing type 2 diabetes. This includes following a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while limiting the intake of sugary and processed foods. A dietitian or healthcare professional can provide personalized guidance on portion sizes, carbohydrate counting, and meal planning. Regular physical activity, such as brisk walking or aerobic exercises, helps improve insulin sensitivity and blood sugar control. Engaging in at least 150 minutes of moderate-intensity aerobic activity per week, along with strength training exercises, is recommended. Weight management is also essential, as losing excess weight can significantly improve diabetes management and insulin sensitivity.
Medication and Insulin Therapy
In addition to lifestyle modifications, many individuals with type 2 diabetes require medication to manage their blood glucose levels effectively. Oral medications, such as metformin, sulfonylureas, and DPP-4 inhibitors, are commonly prescribed to lower blood sugar levels and improve insulin function. In some cases, insulin therapy may be necessary to achieve optimal blood glucose control. Insulin can be administered using insulin pens or syringes, insulin pumps, or inhalers, depending on individual needs. Adherence to prescribed medications, proper timing, and dosage are critical for optimal management.
Blood Sugar Monitoring
Regular monitoring of blood sugar levels is crucial for individuals with type 2 diabetes. This helps determine the effectiveness of treatment plans, identify patterns and trends in blood sugar levels, and make necessary adjustments to medication, diet, and physical activity. Blood sugar monitoring can be done using a glucometer at home or by visiting healthcare facilities for laboratory tests. Healthcare professionals can provide guidance on the frequency and timing of blood sugar testing based on individual needs.
Emotional and Psychological Impact of Type 2 Diabetes
Living with type 2 diabetes not only affects the physical health of individuals but also has a significant impact on their emotional and psychological well-being. Receiving a diagnosis of type 2 diabetes can bring about a range of emotions, including fear, frustration, and sadness. It is important to recognize and address the emotional and psychological aspects of living with this condition in order to maintain a positive outlook and overall quality of life.
Coping with the Diagnosis
Receiving a type 2 diabetes diagnosis can evoke various emotions, including fear, frustration, and sadness. It is important for patients and caregivers to acknowledge these feelings and seek support from healthcare professionals, support groups, and loved ones. Education about the condition and available resources can empower individuals to effectively manage their emotional well-being. Learning about diabetes management, connecting with others who have similar experiences, and engaging in self-care activities, such as practicing mindfulness or engaging in hobbies, can help individuals cope with the diagnosis.
Lifestyle Challenges and Emotional Well-being
Living with type 2 diabetes requires constant attention and adaptation, which can sometimes lead to feelings of stress and anxiety. Balancing dietary restrictions, medication schedules, physical activity, and social engagements can be overwhelming. It is important to prioritize self-care and establish a support system that includes healthcare professionals, family, and friends. Seeking support from healthcare professionals, engaging in stress-reduction techniques (e.g., deep breathing exercises, meditation, yoga), and maintaining a strong support network can alleviate emotional burdens.
Living with type 2 diabetes involves an evolving journey with unique challenges at each stage. Understanding the progression of the disease, managing lifestyle modifications, and addressing emotional well-being are vital aspects of maintaining a high quality of life. By adopting a proactive approach, diabetic patients and their caregivers can navigate this journey successfully. Regular communication with healthcare professionals, adherence to treatment plans, and access to educational resources can empower individuals to live well with type 2 diabetes.