Sleep plays a crucial role in maintaining overall health and well-being, especially for individuals with diabetes. Unfortunately, many people with diabetes often experience sleep-related issues that can negatively impact their quality of life and disease management. In such cases, seeking professional help becomes essential to address these sleep problems effectively. This article aims to provide comprehensive information on the importance of professional help for sleep-related issues in individuals with diabetes, along with practical guidance and resources for both diabetic patients and their caregivers.
The Importance of Sleep for Diabetic Patients
Quality sleep is essential for everyone, but it holds particular significance for individuals with diabetes. Several studies have shown a bidirectional relationship between diabetes and sleep disturbances, with each condition influencing the other. Inadequate sleep can contribute to the development of diabetes and worsen glycemic control in individuals already diagnosed with the disease. On the other hand, diabetes and its associated complications can disrupt sleep patterns and lead to various sleep disorders. Understanding the impact of sleep on diabetes management is crucial for individuals and their caregivers to prioritize sleep health.
Common Sleep-Related Issues in Diabetes
- Insomnia: Insomnia is a sleep disorder characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep. Many diabetic patients report insomnia symptoms, which can be attributed to factors such as hyperglycemia, neuropathy, nocturia (frequent urination at night), and anxiety related to diabetes management. Insomnia can significantly affect daytime functioning, worsen glycemic control, and contribute to the risk of developing other chronic conditions.
- Obstructive Sleep Apnea (OSA): OSA is a prevalent sleep disorder in which breathing is repeatedly interrupted during sleep due to partial or complete airway blockages. Research has indicated a strong association between diabetes and OSA. The shared risk factors between the two conditions, such as obesity and insulin resistance, contribute to this link. OSA can lead to excessive daytime sleepiness, impaired glucose metabolism, and increased cardiovascular risk in individuals with diabetes.
- Restless Legs Syndrome (RLS): RLS is characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations. Although the exact cause of RLS is unknown, studies have shown a higher prevalence of RLS in individuals with diabetes compared to the general population. RLS can disrupt sleep onset and maintenance, leading to fragmented sleep and daytime fatigue.
- Shift Work Sleep Disorder (SWSD): Many individuals with diabetes, especially those in essential occupations, may work in shifts that disrupt their natural sleep-wake cycles. This can result in SWSD, a circadian rhythm sleep disorder characterized by difficulty sleeping during desired sleep times and excessive sleepiness or insomnia during work hours. SWSD can disrupt glycemic control, increase the risk of cardiovascular events, and exacerbate the symptoms of diabetes.
The Role of Professionals in Addressing Sleep Issues
Seeking professional help is crucial when sleep-related issues arise in individuals with diabetes. Healthcare providers with expertise in sleep medicine can offer specialized care, diagnose sleep disorders accurately, and design tailored treatment plans. The following professionals may be involved in managing sleep-related issues in diabetic patients:
- Sleep Medicine Physicians: These medical professionals specialize in the diagnosis and treatment of sleep disorders. They conduct thorough evaluations, including detailed medical history reviews, physical examinations, and may order sleep studies (polysomnography) to assess sleep patterns accurately. Based on the findings, sleep medicine physicians develop personalized treatment strategies.
- Diabetologists/Endocrinologists: Diabetologists and endocrinologists play a vital role in managing diabetes and its associated complications. They collaborate with sleep medicine specialists to ensure comprehensive care for individuals with sleep-related issues. These healthcare professionals focus on optimizing glycemic control, adjusting medications if necessary, and monitoring the impact of sleep disorders on diabetes management.
- Psychologists/Counselors: Psychological factors, such as stress, anxiety, and depression, can contribute to sleep disturbances in individuals with diabetes. Psychologists or counselors with expertise in sleep-related issues can provide cognitive-behavioral therapy for insomnia (CBT-I) and other evidence-based therapies to address these psychological factors and improve sleep quality.
Diagnostic Process and Treatment Options
When seeking professional help for sleep-related issues, a systematic diagnostic process is typically followed to identify the underlying causes accurately. This process may involve the following steps:
- Medical History and Evaluation: The healthcare provider will conduct a detailed medical history review, including diabetes management, sleep patterns, and any associated symptoms. They may also assess the impact of sleep disturbances on the patient’s quality of life and diabetes management.
- Physical Examination: A thorough physical examination may be performed to identify any physical conditions or risk factors that could contribute to sleep-related issues.
- Sleep Study (Polysomnography): In some cases, a sleep study may be recommended to monitor various physiological parameters during sleep. Polysomnography involves non-invasive measurements of brain activity, eye movements, muscle tone, and respiratory patterns. This test helps in diagnosing sleep disorders such as OSA and RLS.
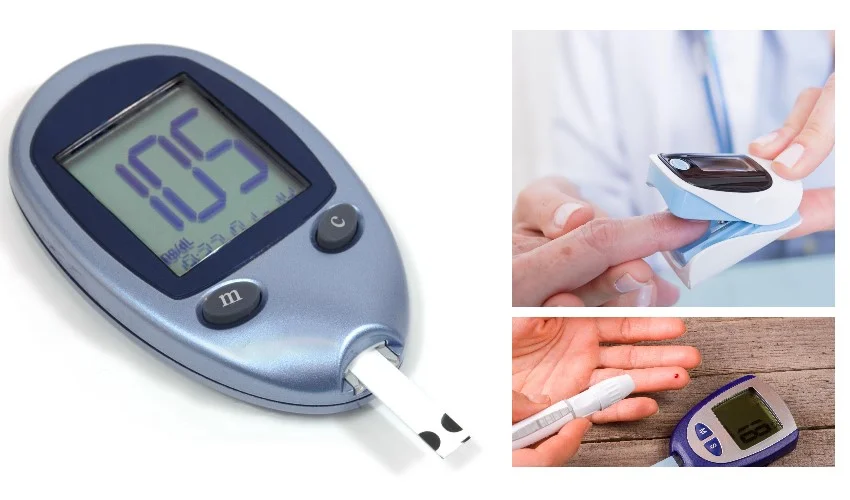
- Blood Glucose Monitoring: For diabetic patients, monitoring blood glucose levels during sleep can provide valuable information regarding the impact of sleep disorders on glycemic control.
Once a diagnosis is established, appropriate treatment options can be considered. Treatment plans are tailored to address the specific sleep disorder and its impact on diabetes management. Here are some commonly used treatment options:
- Continuous Positive Airway Pressure (CPAP): CPAP therapy is the gold standard treatment for obstructive sleep apnea. It involves wearing a mask connected to a machine that delivers a constant flow of air to keep the airway open during sleep.
- Oral Appliances: For individuals with mild to moderate OSA or those who cannot tolerate CPAP, oral appliances can be considered. These devices reposition the jaw and tongue to prevent airway blockages during sleep.
- Medications: In some cases, medications may be prescribed to manage specific sleep disorders. For example, medications that increase dopamine levels in the brain can be effective in treating restless legs syndrome.
- Cognitive-Behavioral Therapy for Insomnia (CBT-I): CBT-I is a non-pharmacological treatment for insomnia that focuses on improving sleep habits, addressing negative thoughts about sleep, and implementing relaxation techniques.
Lifestyle Modifications and Sleep Hygiene Tips
In addition to professional interventions, certain lifestyle modifications and sleep hygiene practices can significantly improve sleep quality for diabetic patients. These include:
- Maintaining a Consistent Sleep Schedule: Establishing a regular sleep schedule by going to bed and waking up at consistent times helps regulate the body’s internal clock and promotes better sleep.
- Creating a Sleep-Friendly Environment: Ensure the sleep environment is dark, quiet, and comfortable. Use blackout curtains, earplugs, or white noise machines if necessary.
- Regular Physical Activity: Engaging in regular physical activity can improve sleep quality and overall health. However, it is important to exercise earlier in the day and avoid intense workouts close to bedtime.
- Healthy Eating Habits: A balanced diet that includes whole grains, lean proteins, fruits, and vegetables promotes good sleep. Avoid heavy meals, caffeine, and alcohol close to bedtime, as they can disrupt sleep patterns.
- Stress Management: Stress can negatively impact sleep quality. Practicing stress management techniques such as meditation, deep breathing exercises, and relaxation techniques can help promote better sleep.
- Limiting Screen Time: The blue light emitted by electronic devices can interfere with sleep. It is advisable to limit screen time, especially before bedtime.
Sleep-related issues can significantly impact the health and well-being of individuals with diabetes. Seeking professional help is crucial to accurately diagnose and effectively manage these sleep problems. By consulting healthcare professionals with expertise in sleep medicine and collaborating with dialectologists or endocrinologists, individuals with diabetes can receive comprehensive care to improve their sleep quality, glycemic control, and overall quality of life. It is also important to incorporate lifestyle modifications and practice good sleep hygiene to optimize sleep health. By addressing sleep-related issues, individuals with diabetes can better manage their condition and enhance their overall well-being.