Living with diabetes can present various challenges, including pain and discomfort. Managing diabetes-related pain is crucial for enhancing the quality of life for individuals with diabetes. In this article, we will explore the different types of pain and discomfort experienced by people with diabetes, understand their underlying causes, and discuss effective solutions to alleviate and manage these symptoms. By implementing appropriate strategies, individuals with diabetes and their caregivers can improve their overall well-being and enhance their daily lives.
Understanding Diabetes-Related Pain and Discomfort
Living with diabetes often involves experiencing pain and discomfort that can significantly impact an individual’s quality of life. Let’s explore the various types of pain and discomfort commonly associated with diabetes and understand their underlying causes.
Types of Pain and Discomfort
Living with diabetes can often involve experiencing various types of pain and discomfort. Diabetes is a chronic condition that affects the body’s ability to regulate blood sugar levels, leading to a range of complications that can cause discomfort and pain. Here are some common types of pain and discomfort associated with diabetes:
Neuropathic Pain
Neuropathic pain is one of the most prevalent types of pain experienced by individuals with diabetes. It results from nerve damage caused by high blood sugar levels over time. Common neuropathic pain symptoms include tingling, burning, shooting, or stabbing sensations, often affecting the feet and hands.
Neuropathic pain can be challenging to manage and may require a multidimensional approach for effective relief.
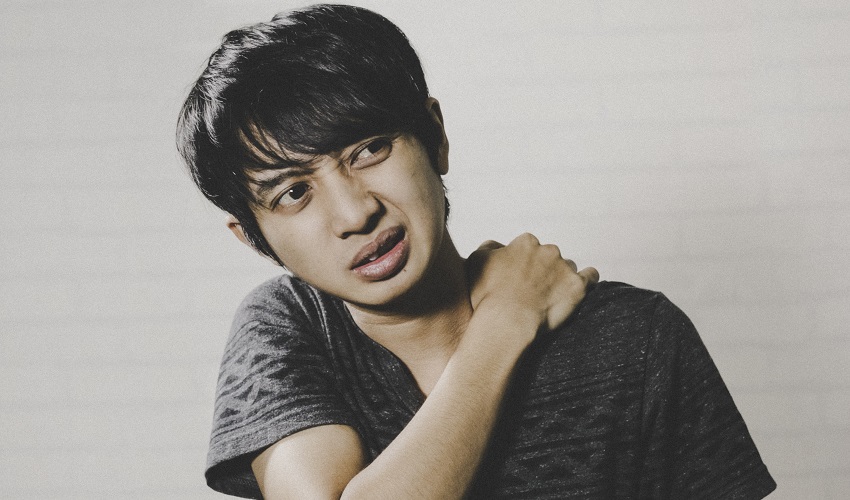
Musculoskeletal Pain
Musculoskeletal pain refers to pain in the muscles, joints, bones, and tendons. People with diabetes may experience musculoskeletal pain due to factors such as poor circulation, diabetic neuropathy, or complications like frozen shoulder, carpal tunnel syndrome, or Dupuytren’s contracture.
Musculoskeletal pain can significantly impact daily activities and mobility, making it essential to address and manage appropriately.
Vascular Pain
Vascular pain arises from the impairment of blood flow and circulation. Peripheral arterial disease (PAD) is a common vascular condition in diabetes that can cause pain, particularly in the legs and feet. Pain associated with PAD is often described as cramping, aching, or heaviness.
Proper management of vascular pain is crucial for improving blood flow and preventing complications.
Dental and Oral Pain
Diabetes can also lead to dental and oral complications, resulting in pain and discomfort. Gum disease, oral infections, and dry mouth are common problems experienced by individuals with diabetes, leading to oral pain and difficulty in eating and speaking.
Effective oral hygiene practices and regular dental check-ups are essential for managing dental pain and maintaining oral health.
Causes of Diabetes-Related Pain and Discomfort
Diabetes-related pain and discomfort are often overlooked aspects of the disease. Understanding the causes of these issues is crucial for both individuals with diabetes and healthcare professionals. By addressing the underlying causes and implementing appropriate treatment strategies, it is possible to alleviate pain and improve the overall quality of life for those living with diabetes. Regular monitoring, maintaining blood sugar levels, and adopting a comprehensive management plan can help mitigate the impact of diabetes-related pain and discomfort.
Diabetic Neuropathy
Diabetic neuropathy is a condition characterized by nerve damage resulting from prolonged high blood sugar levels. It is a leading cause of pain and discomfort in individuals with diabetes. The damage can affect sensory, motor, or autonomic nerves, leading to various symptoms, including pain, numbness, tingling, and loss of sensation.
The prevention and management of diabetic neuropathy involve maintaining good blood sugar control, adopting a healthy lifestyle, and implementing targeted treatment strategies.
Peripheral Arterial Disease (PAD)
Peripheral arterial disease occurs when blood vessels become narrow or blocked, resulting in reduced blood flow to the extremities. PAD can cause pain, cramping, and discomfort, particularly during physical activity or when resting.
Lifestyle modifications, medication management, and, in severe cases, interventional procedures are key to managing vascular pain associated with PAD.
Charcot Foot
Charcot foot is a severe complication of diabetic neuropathy that weakens the bones in the foot. It can lead to foot deformities, instability, and chronic pain.
Early detection, proper foot care, and regular podiatric care are essential for preventing and managing Charcot foot.
Dental and Oral Complications
Individuals with diabetes are more susceptible to oral health issues, including gum disease, tooth decay, and dry mouth. These complications can cause oral pain and discomfort.
Maintaining good oral hygiene practices, seeking regular dental check-ups, and following recommended treatments can help manage dental pain and prevent further complications.
Managing Neuropathic Pain in Diabetes
Neuropathic pain is a common and challenging symptom for individuals with diabetes. Proper management strategies are essential for alleviating pain and improving daily functioning.
Types of Diabetic Neuropathy
Diabetic neuropathy is a common and potentially debilitating complication of diabetes mellitus. It is a nerve disorder that can affect various parts of the body, resulting in a wide range of symptoms. Diabetic neuropathy is primarily caused by prolonged high blood sugar levels, which can damage the small blood vessels that supply the nerves.
There are several types of diabetic neuropathy, each with its own distinct set of symptoms and areas of the body it affects. Understanding these different types is crucial for individuals living with diabetes, as early detection and management can help prevent further complications and improve overall quality of life.
Peripheral Neuropathy
Peripheral neuropathy affects the peripheral nerves, leading to symptoms such as tingling, numbness, burning, or shooting pain, usually in the feet and hands.
Autonomic Neuropathy
Autonomic neuropathy affects the nerves that control involuntary body functions, such as digestion, heart rate, and blood pressure. It can cause symptoms like gastrointestinal problems, dizziness, and difficulty in bladder control.
Proximal Neuropathy
Proximal neuropathy primarily affects the nerves in the hips, thighs, buttocks, and legs, leading to pain, weakness, and difficulty in movement.
Symptoms and Risk Factors
The symptoms of diabetic neuropathy can vary depending on the type and nerves affected. Common symptoms include pain, numbness, tingling, weakness, and balance problems. Risk factors for developing neuropathy include prolonged diabetes duration, poor blood sugar control, smoking, and obesity.
Management Strategies
Managing diabetic neuropathy involves a comprehensive approach to control blood sugar levels, relieve pain, and prevent further nerve damage.
Glycemic Control
Maintaining good blood sugar control is essential for preventing and managing neuropathic pain. Monitoring blood sugar levels regularly, adhering to a diabetes-friendly diet, and taking prescribed medications as directed are key components of glycemic control.
Medications for Neuropathic Pain
Several medications, such as anticonvulsants, antidepressants, and topical creams, can help alleviate neuropathic pain. These medications work by targeting the nerves and reducing pain signals.
Physical Therapy and Exercise
Physical therapy exercises can improve strength, balance, and coordination, reducing the risk of falls and managing pain. Low-impact exercises like walking, swimming, and cycling are particularly beneficial.
Alternative Therapies
Complementary and alternative therapies like acupuncture, transcutaneous electrical nerve stimulation (TENS), and biofeedback may provide additional pain relief for some individuals. However, it’s important to consult healthcare professionals before incorporating these therapies.
Addressing Musculoskeletal Pain in Diabetes
Musculoskeletal pain is a common complaint among individuals with diabetes. Understanding the causes and implementing appropriate management strategies can alleviate discomfort and improve daily functioning.
Causes and Risk Factors
Musculoskeletal pain in diabetes can result from various factors, including poor circulation, nerve damage, inflammation, and joint stiffness. Additionally, specific musculoskeletal conditions are more prevalent in individuals with diabetes.
Common Musculoskeletal Conditions in Diabetes
Musculoskeletal conditions can significantly impact the quality of life and functional abilities of individuals living with diabetes. Regular monitoring and early intervention are crucial to managing these conditions effectively. Proper glycemic control, exercise, and multidisciplinary care involving endocrinologists, podiatrists, physiotherapists, and hand specialists play a vital role in preventing and managing musculoskeletal complications in people with diabetes.
Frozen Shoulder
Frozen shoulder, also known as adhesive capsulitis, causes pain and stiffness in the shoulder joint. Individuals with diabetes have a higher risk of developing this condition, which can restrict shoulder movement and cause discomfort.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is a condition that causes pain, tingling, and numbness in the hand and fingers due to compression of the median nerve. Diabetes can increase the risk of developing carpal tunnel syndrome.
Dupuytren’s Contracture
Dupuytren’s contracture is a condition in which the tissues beneath the skin of the palm and fingers thicken and tighten, causing the fingers to bend inward. It can lead to pain and limited hand function.
Management Strategies
Managing musculoskeletal pain in diabetes involves a combination of medical interventions, lifestyle modifications, and self-care strategies.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics, and muscle relaxants may be prescribed to alleviate musculoskeletal pain. These medications can provide temporary relief and improve daily functioning.
Physical Therapy
Physical therapy plays a vital role in managing musculoskeletal pain. Therapeutic exercises, stretching, and manual techniques can improve joint mobility, reduce pain, and strengthen muscles.
Assistive Devices
Using assistive devices such as braces, splints, or orthotics can provide support, stability, and pain relief for affected joints.
Heat and Cold Therapy
Applying heat or cold to the affected areas can help reduce pain and inflammation. Heat therapy promotes blood flow and relaxation, while cold therapy numbs the area and reduces swelling.
Managing Vascular Pain Associated with Peripheral Arterial Disease (PAD)
Peripheral arterial disease is a common vascular complication in diabetes, causing pain and discomfort. Understanding PAD, its symptoms, and treatment options is crucial for managing vascular pain effectively.
Peripheral Arterial Disease (PAD): An Overview
PAD occurs when arteries supplying blood to the legs and feet become narrowed or blocked due to atherosclerosis. Reduced blood flow can lead to pain, cramping, and discomfort, particularly during physical activity or when resting.
Symptoms and Risk Factors
Common symptoms of PAD include leg pain, cramping, numbness, weakness, and slow-healing foot sores. Risk factors for PAD include diabetes, smoking, high blood pressure, high cholesterol, and obesity.
Treatment Approaches
Managing vascular pain associated with PAD involves lifestyle modifications, medications, and, in some cases, interventional procedures.
Lifestyle Modifications
Lifestyle changes play a vital role in managing PAD. These may include quitting smoking, adopting a heart-healthy diet low in saturated fats and cholesterol, engaging in regular exercise, maintaining a healthy weight, and managing other coexisting conditions such as diabetes and high blood pressure.
Medications
Medications can be prescribed to manage the symptoms of PAD, lower blood pressure and cholesterol levels, prevent blood clot formation, and improve blood flow.
Interventional Procedures
In advanced cases of PAD, interventional procedures such as angioplasty, stenting, or bypass surgery may be required to restore blood flow and alleviate pain.
Preventive Measures
Prevention is key in managing vascular pain associated with PAD. Regular check-ups, early detection of PAD, and adherence to prescribed treatments and lifestyle modifications can help prevent or delay the progression of the condition.
Dental and Oral Complications in Diabetes
Diabetes can significantly impact oral health, leading to dental complications and associated pain and discomfort. Understanding these complications and implementing proper dental care practices are crucial for managing oral pain effectively.
Oral Health Issues Associated with Diabetes
Individuals with diabetes are more prone to dental problems due to factors such as reduced saliva production, compromised immune function, and elevated glucose levels in saliva.
Common Dental Complications
Diabetes can contribute to gum disease (periodontitis), tooth decay, dry mouth (xerostomia), oral infections, and delayed wound healing in the mouth. These conditions can cause oral pain, difficulty in chewing and swallowing, and impact overall oral health.
Dental Pain Management
Adopting good oral hygiene practices and seeking regular dental care are essential for managing dental pain and preventing complications.
Oral Hygiene Practices
Maintaining excellent oral hygiene by brushing teeth at least twice a day with a soft-bristled toothbrush, flossing daily, and using an antibacterial mouthwash can prevent gum disease, tooth decay, and oral infections.
Regular Dental Check-ups
Regular dental check-ups allow for early detection and treatment of oral complications. Dental professionals can provide professional cleaning, oral health assessment, and advice on managing specific dental issues.
Treatment of Dental Complications
Seeking timely treatment for dental complications such as gum disease, tooth decay, or oral infections is crucial for pain management and preventing further damage.
Managing diabetes-related pain and discomfort is essential for enhancing the quality of life for individuals with diabetes. By understanding the different types of pain, their causes, and implementing effective management strategies, individuals with diabetes and their caregivers can significantly improve their daily lives. Regular healthcare check-ups, adherence to prescribed treatments, lifestyle modifications, and proper self-care practices are key steps towards managing pain and discomfort associated with diabetes. Remember, early detection and proactive management are crucial for a healthier and more comfortable life with diabetes.