Living with diabetes can be challenging, requiring a comprehensive approach to managing the condition effectively. While conventional medical treatments play a crucial role in diabetes management, exploring alternative treatments and complementary therapies can provide additional support to improve overall well-being. In this article, we will delve into various alternative treatments and complementary therapies that can be considered by diabetic patients and their caregivers. By understanding these options, individuals can make informed decisions in consultation with their healthcare providers.
Understanding Alternative Treatments and Complementary Therapies
Alternative treatments and complementary therapies are non-conventional approaches that can be used alongside conventional medical treatments to manage diabetes. While they should not replace medical advice, they can offer additional support and improve overall well-being. It is essential to understand that alternative treatments should always be discussed with healthcare providers to ensure their safety and compatibility with existing treatment plans.
Dietary Interventions for Diabetes Management
Proper nutrition plays a vital role in diabetes management. Several dietary interventions have shown promising results in controlling blood sugar levels and reducing the risk of complications.
Low-Carbohydrate Diet
A low-carbohydrate diet restricts the intake of high glycemic index foods, such as refined sugars and grains, and encourages the consumption of non-starchy vegetables, lean proteins, and healthy fats. Research suggests that low-carbohydrate diets can improve blood glucose control and promote weight loss in individuals with diabetes.
One study published in the Journal of the American Medical Association (JAMA) compared the effects of a low-carbohydrate diet and a low-fat diet on glycemic control in individuals with type 2 diabetes. The study found that the low-carbohydrate diet group experienced greater improvements in hemoglobin A1c levels, indicating better long-term glucose control, compared to the low-fat diet group. Additionally, the low-carbohydrate diet group showed greater reductions in triglycerides and higher levels of high-density lipoprotein (HDL) cholesterol, which are favorable for cardiovascular health.
Mediterranean Diet
The Mediterranean diet emphasizes whole grains, fruits, vegetables, legumes, nuts, and olive oil while limiting red meat and processed foods. Studies have shown that following a Mediterranean diet can improve glycemic control, reduce cardiovascular risk factors, and lower the incidence of complications in individuals with diabetes.
A systematic review and meta-analysis published in the American Journal of Clinical Nutrition analyzed the effects of the Mediterranean diet on glycemic control and cardiovascular risk factors in individuals with type 2 diabetes. The review found that adherence to the Mediterranean diet was associated with significant reductions in hemoglobin A1c levels, fasting blood glucose, and total cholesterol levels.
Plant-Based Diet
A plant-based diet focuses on consuming whole foods derived from plants, including fruits, vegetables, legumes, whole grains, and nuts, while minimizing or eliminating animal products. Research indicates that a plant-based diet can lead to improved insulin sensitivity, weight management, and cardiovascular health for individuals with diabetes.
A study published in the Journal of Geriatric Cardiology compared the effects of a low-fat plant-based diet and a conventional diabetes diet in individuals with type 2 diabetes. The study found that the plant-based diet group experienced greater reductions in hemoglobin A1c levels and improved insulin sensitivity compared to the conventional diabetes diet group.
Herbal and Nutritional Supplements
Herbal and nutritional supplements have gained attention for their potential benefits in diabetes management. It is important to note that these supplements should not replace prescribed medications but can complement conventional treatments. Some supplements that have shown promise in diabetes management include:
- Alpha-Lipoic Acid (ALA): ALA has demonstrated antioxidant properties and potential benefits in improving insulin sensitivity and reducing neuropathic symptoms in diabetic patients.
- Cinnamon: Studies suggest that cinnamon may help improve insulin sensitivity and reduce blood glucose levels in individuals with type 2 diabetes.
- Chromium: Chromium is involved in carbohydrate and lipid metabolism and may contribute to better glycemic control when taken as a supplement.
- Omega-3 Fatty Acids: Omega-3 fatty acids, found in fish oil and certain plant sources, have shown potential in reducing inflammation and improving cardiovascular health in individuals with diabetes.
While these supplements show promise, it is crucial to consult with healthcare providers before starting any new supplements to ensure they are safe and compatible with existing treatment plans.
Mind-Body Therapies
Mind-body therapies focus on the connection between the mind, body, and emotions. They can be valuable tools for stress reduction and improving overall well-being in individuals with diabetes.
Meditation
Meditation involves focusing attention and eliminating the stream of thoughts. Regular meditation practice has been associated with reduced stress levels, improved glycemic control, and enhanced quality of life in individuals with diabetes.
A randomized controlled trial published in the Annals of Family Medicine examined the effects of mindfulness meditation on glycemic control in individuals with type 2 diabetes. The study found that participants who underwent an eight-week mindfulness meditation program experienced significant reductions in hemoglobin A1c levels and improvements in self-care behaviors compared to the control group.
Yoga
Yoga combines physical postures, breathing exercises, and meditation to promote physical and mental well-being. It has shown potential benefits in improving glycemic control, reducing stress, and enhancing flexibility and strength in individuals with diabetes.
A systematic review and meta-analysis published in the journal PLOS ONE evaluated the effects of yoga on glycemic control in individuals with type 2 diabetes. The review found that practicing yoga was associated with significant reductions in fasting blood glucose levels and hemoglobin A1c levels.
Tai Chi
Tai Chi is an ancient Chinese martial art that involves slow and gentle movements, deep breathing, and focused attention. Studies have shown that Tai Chi can improve glycemic control, balance, and overall quality of life in individuals with diabetes.
A meta-analysis published in the journal PLOS ONE analyzed the effects of Tai Chi on glycemic control in individuals with type 2 diabetes. The analysis revealed that practicing Tai Chi was associated with significant reductions in hemoglobin A1c levels and improvements in insulin resistance.
Acupuncture and Acupressure
Acupuncture and acupressure are traditional Chinese therapies that involve the stimulation of specific points on the body. These practices aim to restore the flow of energy, known as Qi, and promote overall health. Some studies suggest that acupuncture and acupressure may help improve insulin sensitivity and alleviate diabetes-related symptoms, such as neuropathy.
A systematic review published in the journal Diabetes Research and Clinical Practice examined the effects of acupuncture on glycemic control in individuals with diabetes. The review concluded that acupuncture showed potential benefits in reducing fasting blood glucose levels and improving insulin sensitivity.
Massage Therapy
Massage therapy involves the manipulation of soft tissues in the body to promote relaxation and relieve muscle tension. While research on massage therapy specifically for diabetes management is limited, it may contribute to stress reduction, improved blood circulation, and overall well-being.
A study published in the journal Diabetes Spectrum explored the effects of massage therapy on blood glucose levels in individuals with type 2 diabetes. The study found that participants who received regular massage sessions experienced reductions in fasting blood glucose levels and perceived stress.
Physical Activity and Exercise
Regular physical activity and exercise are essential components of diabetes management. Engaging in aerobic exercises, strength training, and flexibility exercises can help improve insulin sensitivity, maintain a healthy weight, reduce cardiovascular risk factors, and enhance overall well-being.
The American Diabetes Association recommends a combination of aerobic exercises (such as brisk walking, swimming, or cycling), strength training exercises, and flexibility exercises for individuals with diabetes. It is important to consult with healthcare providers to develop an exercise plan tailored to individual needs and capabilities.
Important Considerations and Precautions
When considering alternative treatments and complementary therapies, it is crucial to keep the following in mind:
- Always consult with healthcare providers to understand what kind of doctor treats diabetes before starting any new treatment or therapy.
- Inform healthcare providers about all supplements and therapies being used to ensure compatibility with prescribed medications.
- Be cautious of misleading claims or unproven treatments that promise a “cure” for diabetes.
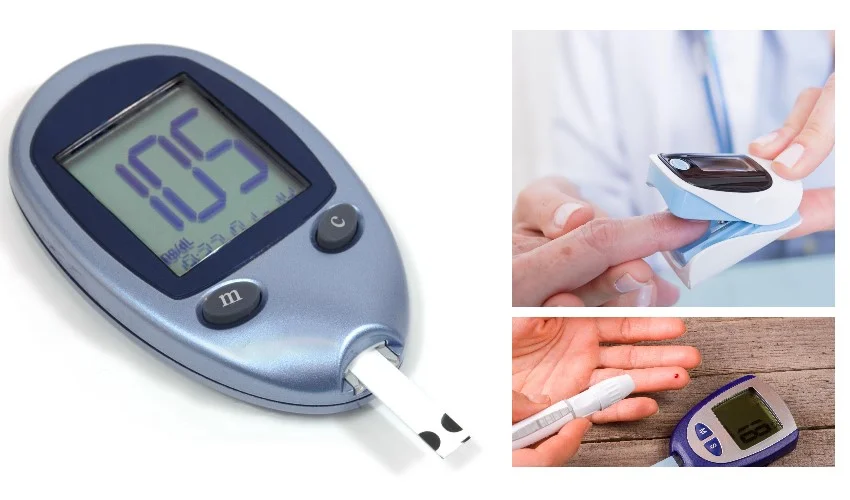
- Monitor blood glucose levels regularly and adjust treatment plans as necessary.
- Complementary therapies should be seen as additional support and not as a substitute for conventional medical care.
Exploring alternative treatments and complementary therapies can provide additional avenues for diabetic patients and their caregivers to improve overall well-being and enhance diabetes management. While these treatments should not replace conventional medical care, they can be valuable complements to existing treatment plans. By discussing these options with healthcare providers and considering evidence-based approaches, individuals can make informed decisions to optimize their diabetes management journey.