Most discussions around diabetes focus on insulin resistance, diet, and exercise. However, one crucial factor remains largely unexplored: the role of gut microbiota in diabetes onset, progression, and management. Research is beginning to disclose new insights into how the trillions of bacteria living in our digestive system can influence blood sugar levels, insulin sensitivity, and even inflammation. This research provides useful new insights about diabetes, which is helpful in the prevention and treatment of new cases of the disease.
What is Gut Microbiota?
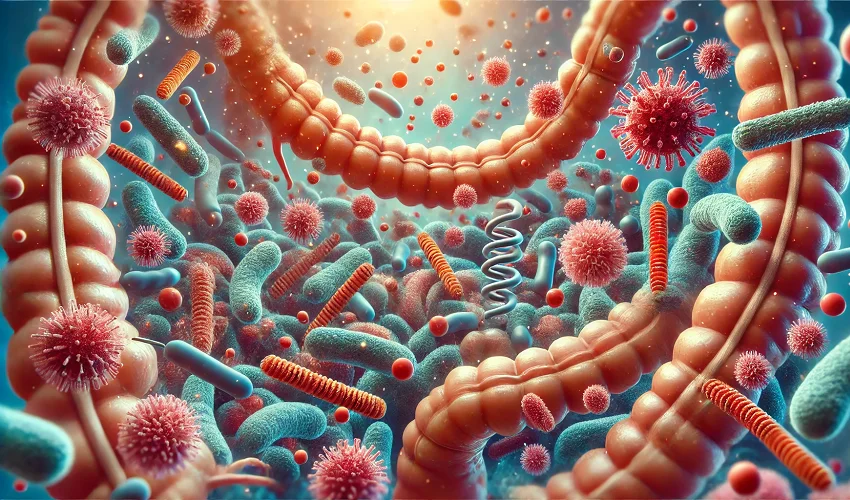
The gut microbiota includes a range of microorganisms. They include bacteria, fungi, and viruses, that reside in your intestines. These microbes help in digestion process, immune functioning, and your overall metabolic health. If your gut microbiome is balanced, it helps in proper absorption of nutrients that are essential for the body and also in the production of key metabolites like short-chain fatty acids (SCFAs). Eventually, this affects how the body regulates insulin function and glucose metabolism in the body.
How Gut Microbiota Affects Diabetes
According to a recent research that was published in The Cureus Journal of Medical Science in 2023 [1], the gut microbiota significantly had a relationship in diabetic individuals, which showed consistent patterns of alterations in SCFA, modified bile acid metabolism, altered lipopolysaccharides, changes in bacterial compositions, and energy producers.
These are some ways gut microbiota can affect individuals with diabetes.
Influence on Insulin Sensitivity:
- Studies suggest that individuals with type 2 diabetes often have an imbalance in gut bacteria. This is known as dysbiosis. Some bacterial strains may also promote inflammation and reduce insulin sensitivity, which ultimately increases the risk of high blood sugar levels.
Regulation of Blood Sugar Levels
- Gut bacteria influence the breakdown of dietary fiber into SCFAs, such as butyrate. This helps in improving insulin response and glucose control. A deficiency in butyrate-producing bacteria can increase your blood sugar levels.
Impact on Chronic Inflammation
- An imbalance in your gut microbiota can generate triggers for low-grade inflammation by increasing intestinal permeability, called “leaky gut.” This causes harmful toxins to enter your bloodstream which can cause insulin resistance and metabolic disorders.
Connection with Hematochezia and Digestive Issues
- People with diabetes often experience gastrointestinal issues, including constipation, diarrhea, and even rectal bleeding (hematochezia). Dysbiosis may contribute to gut-related complications, which can further influence the progression and management of diabetes in high-risk individuals.
- Artificial sweeteners are a healthy alternative to sugar for diabetic people.
- What to do instead?
- Some studies suggest that artificial sweeteners alter gut microbiota and may contribute to insulin resistance over time.
- Choose natural sweeteners like stevia or focus on reducing overall sugar intake.
Factors That Disrupt Gut Microbiota in Diabetics
- Excessive Sugar and Processed Foods: High consumption of refined sugars and artificial sweeteners changes gut flora and reduces beneficial bacteria in your intestines.
- Antibiotic Overuse: If you are consuming antibiotic frequently, it can wipe out beneficial gut bacteria, leading to dysbiosis.
- Chronic Stress: Long-term stress influences gut microbiota composition and increases inflammation in the body causing insulin resistance.
- Lack of Fiber: Fiber feeds beneficial bacteria and promotes a healthier gut environment. A fiber-deficient diet deprives the microbiota of essential nutrients which helps maintain the health of your body.
Restoring Gut Health for Better Diabetes Management
Increase Probiotic Intake
You should consume probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi to help replenish beneficial gut bacteria.
Eat More Prebiotic Foods
Prebiotics are found in garlic, onions, leeks, and bananas. They feed you with healthy gut bacteria and improve gut diversity.
Reduce Artificial Sweeteners
Many artificial sweeteners negatively impact gut microbiota and you should minimize their consumption.
Consume More Fiber
Soluble fiber, found in oats, legumes, and vegetables promote the production of SCFAs, improving insulin sensitivity.
Manage Stress and Sleep
Chronic stress and poor sleep are linked to diabetes development. Poor sleep disturbs your gut microbiome, which then causes worsening of the metabolic health.


Future of Gut Microbiota Research in Diabetes
With more research and technology advancements, personalized probiotic therapies may become a standard part of diabetes treatment. Scientists are exploring how these microbiome-based interventions, such as fecal transplants and targeted bacterial supplementation, could offer new hope for diabetes management.
The gut microbiota plays a far more significant role in diabetes than previously understood. If we can focus on gut health through diet, probiotics, and lifestyle changes, doctors can better treat individuals and be able to better regulate blood sugar levels and reduce their risk of complications. As science continues to find the intricate relationship between the gut and metabolic health, new treatments and prevention strategies for diabetes may emerge. This is certainly going to revolutionize the way we approach this widespread condition called diabetes.
Trusted Sources:
- Aishwarya Sadagopan, Anas Mahmoud, and Maha Begg et al., “Understanding the Role of the Gut Microbiome in Diabetes and Therapeutics Targeting Leaky Gut: A Systematic Review,” PMC, July 8, 2023.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10405753/